
At Naseem Medical Billing Company, we are dedicated to providing top-notch medical billing services to healthcare providers across the industry. Our mission is to streamline the billing process, ensuring accuracy, efficiency, and compliance, so that healthcare professionals can focus on what they do best – providing exceptional care to their patients.
Founded with a vision to revolutionize medical billing, Naseem Medical Billing Company has grown to become a trusted partner for numerous healthcare providers. Our journey began with a commitment to address the common challenges faced by medical practices, including billing errors, delayed payments, and complex regulatory requirements. Over the years, we have developed a robust system that simplifies these processes and maximizes revenue for our clients.

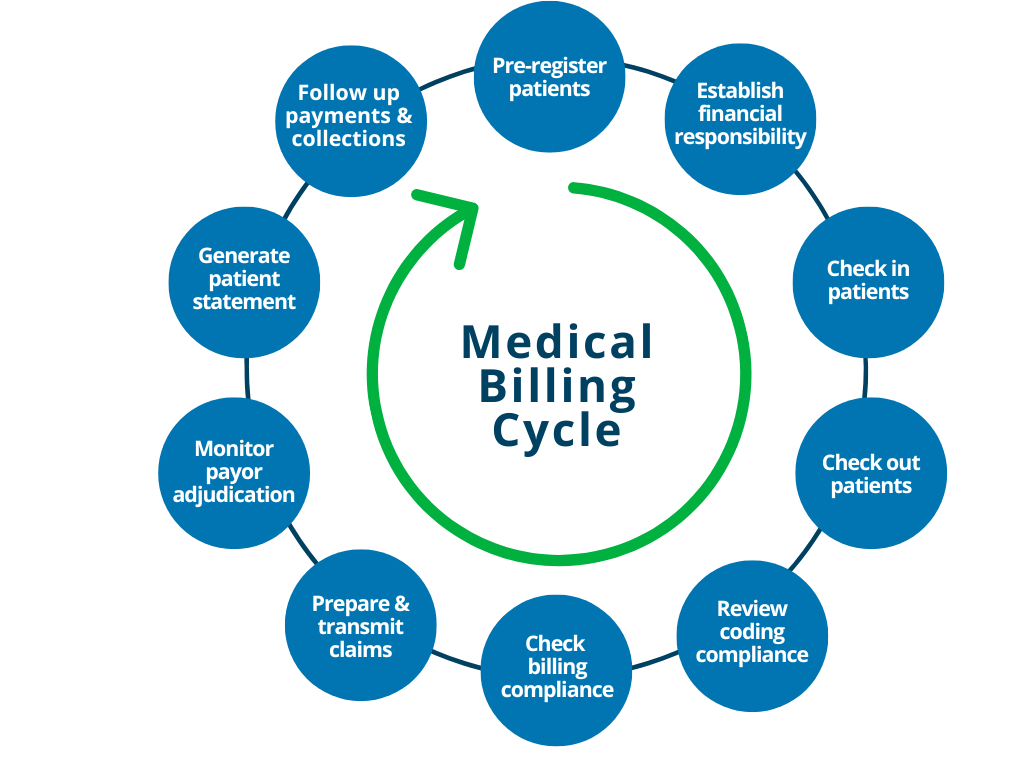
We offer a comprehensive range of services designed to meet the unique needs of healthcare
providers, including:
i. Medical Billing and Coding:
Our team of certified professionals
ensures
accurate and timely billing and coding, reducing claim denials and increasing revenue.
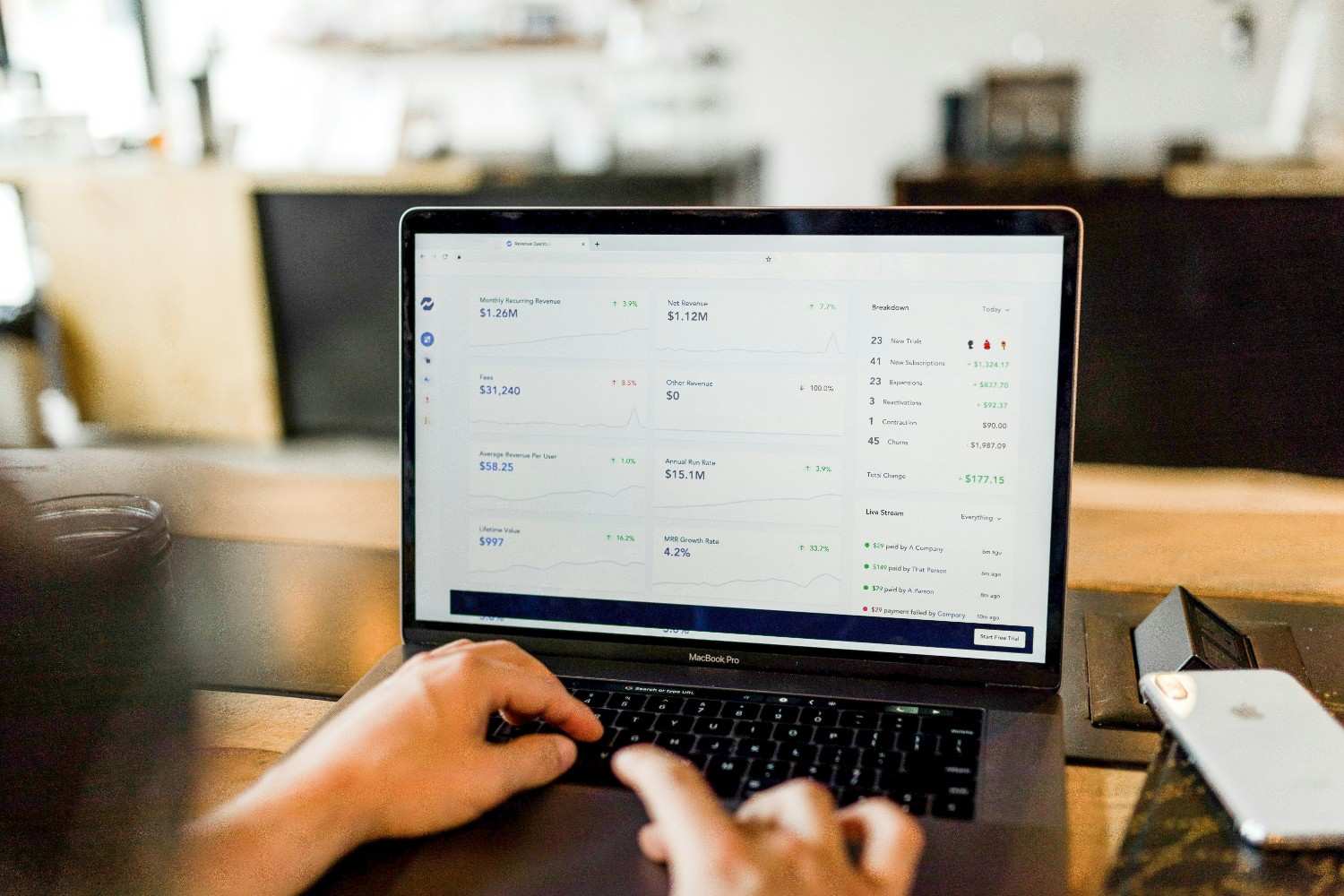
ii. Revenue Cycle Management:
We handle every aspect of the revenue
cycle, from
patient registration to final payment, optimizing your financial performance.
iii. Claims Submission and Follow-Up:
We manage the entire claims
process, from
submission to follow-up, ensuring that you receive timely reimbursements.
iv. Compliance and Audit Support:
Our experts stay updated with the
latest
regulatory changes, providing guidance and support to ensure compliance and minimize audit
risks.
v. Patient Billing Services:
We handle patient billing inquiries and
payments,
offering a seamless and professional experience for your patients.
Naseem Medical Billing and Collection Services focuses on providing comprehensive denial
management to ensure healthcare providers receive accurate and timely reimbursements. Their
denial management process includes several key components:
i Identification and Tracking:
They meticulously track all claims submitted to insurance companies
to identify any denials promptly. This helps in recognizing patterns and preventing future
denials.
ii Categorization of Denials:
Denials are categorized based on the reason codes provided by the
insurers, which helps in understanding the common causes of denials and addressing them
systematically.
iii Analysis and Resolution:
The team analyzes each denial to determine the root cause, whether it
is due to coding errors, missing information, or issues with patient eligibility. They then take
corrective actions, such as updating information, correcting codes, and resubmitting claims.
iv Appeals Management:
For denials that are deemed unjustified, Naseem Medical Billing prepares and
submits appeals to insurance companies, providing the necessary documentation and evidence to
support the claims.
v Reporting and Feedback:
They generate detailed reports on denial trends and resolutions, which
are shared with healthcare providers. This feedback loop helps in continuous improvement of the
billing process and reduces the likelihood of future denials.
vi Staff Training and Updates:
The company ensures that their staff is well-trained and updated
with the latest coding practices, insurance policies, and regulatory changes to minimize errors
and improve the efficiency of claim processing.